Introduction
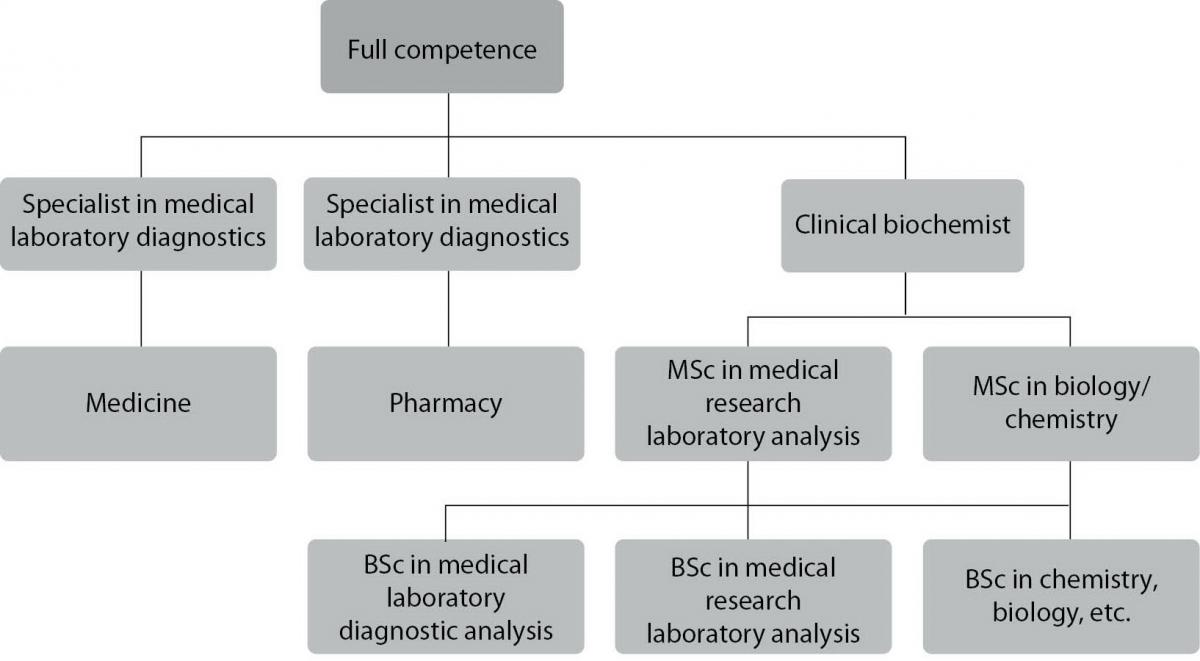
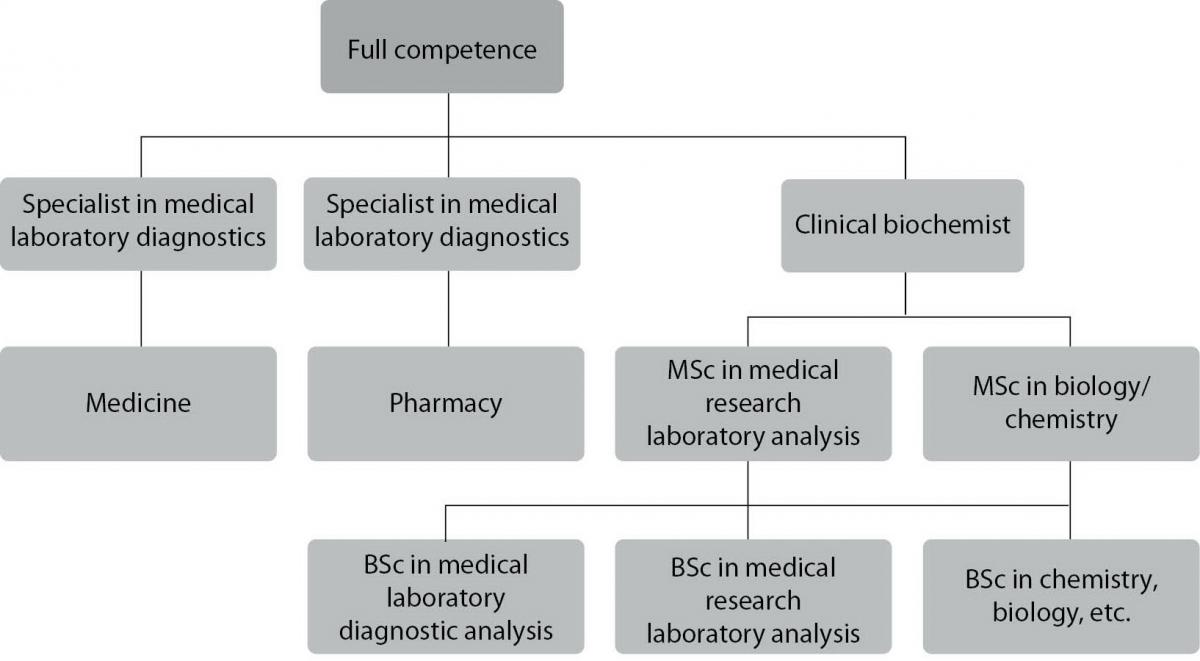
Laboratory medicine in Hungary – like in many other countries – developed as a separate discipline from the 1950s. Until that date clinical laboratories had been organized either as a part of General Pathology Departments or as a specialized unit of Internal Medicine Departments. Nowadays, the number of licensed medical laboratories exceeds 270. Out of them, the 4 medical faculties, located in Budapest, Debrecen, Pécs and Szeged, can boast an Institute of Laboratory Medicine, offering laboratory services together with undergraduate, graduate and postgraduate training of laboratory specialist. They are also involved in basic and clinical research. Approximately another 25 big laboratories located in non-university general hospitals serve as teaching laboratories of the university departments, involved in one or more practical aspects of laboratory training. The current review gives an overview of the principles and practice of the educational system of laboratory specialists in Hungary (Figure 1).
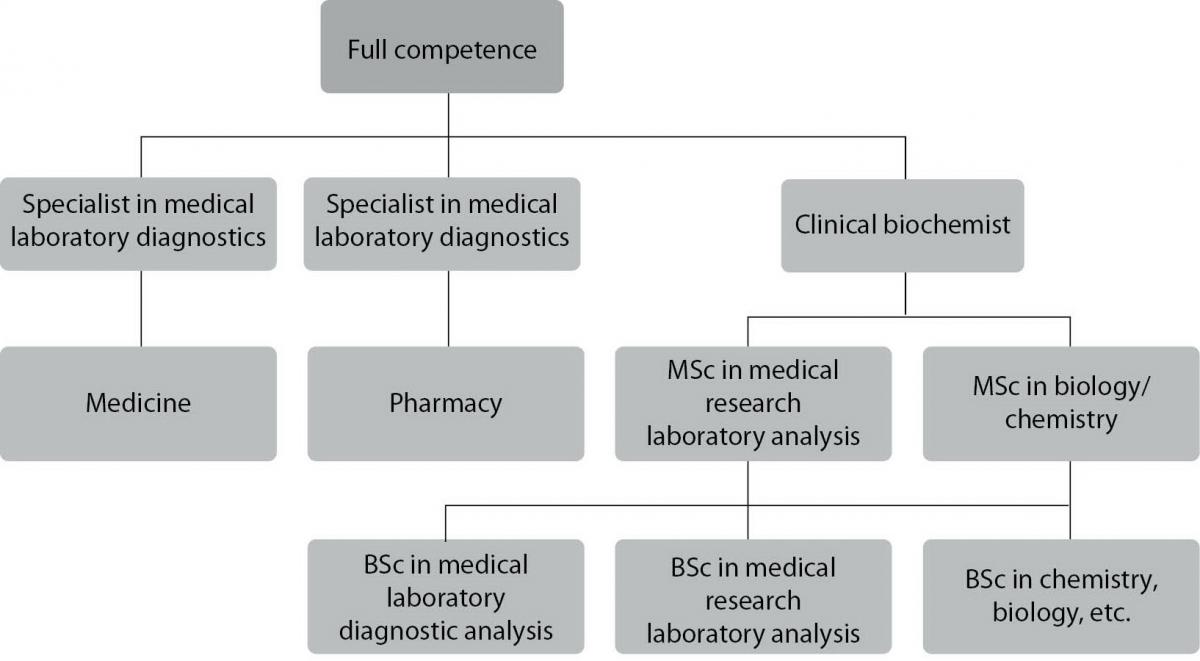
Figure 1. Various training forms in Hungary leading to a fully competent laboratory specialist.
Undergraduate training of medical students
Undergraduate medical students learn clinical biochemistry as an independent core discipline. Clinical biochemistry for medical students in Hungary was first offered at the Pécs Medical University in 1992. The name of the discipline has changed several times, but by now most university medical schools have accepted the term Clinical biochemistry. It is important to declare that clinical biochemistry is an essentially different subject from basic biochemistry or the rather theoretical pathophysiology. The main goal of teaching clinical biochemistry is to develop understanding of, and a critical approach to exact, measured parameters obtained by the analyses of samples taken from patients. At Pécs University Medical School one semester of clinical biochemistry is taught with 14 lecture and 14 seminar hours with a final oral exam at the end of the course. Due to the fact that 2/3 of the medical students come from abroad, we teach clinical biochemistry in Hungarian, English and German languages. At the Debrecen University Medical School, clinical biochemistry is also a core discipline and is taught for third-year medical students in two semesters closing with a final exam. At the Semmelweis Medical University in Budapest teaching clinical biochemistry as an obligatory discipline was launched only in this current academic year. However, at Szeged University Medical School, clinical biochemistry is still taught only as an elective subject. Once graduated from a medical school, young doctors have no special competencies in laboratory medicine (or in any other branches of medicine). They may work in a laboratory under supervision and may register for specialization or scientific training (PhD programs).
Postgraduate specialization of medical doctors: medical laboratory diagnostics
In Hungary, the training of medical specialists is regulated by a government decree. The former, centralized system – offered at the Postgraduate Medical University of Budapest – has dissolved, and since 1999 onwards, the medical universities have been responsible for offering postgraduate medical training schemes. Regionally, Centers for Postgraduate Education were established according to the geographical positions of medical schools, where the medical (and pharmaceutical) graduates enrolled in specialist training are registered and their training is organized. The content and structure of the training is regulated by a decree of the Ministry in charge.
The quality of training for every specialization is guaranteed by an accreditation processes revised every five years. The application is partly based on self-evaluation of the training institution in education/research/patient care, partly on assessment of the staff, infrastructure, instrumentation involved in the training. In Hungary, specialist trainings can be funded by the state, or by the trainee. State-funded training can be run as part of a centrally supported training system (e.g. employment by the university) or in the framework of residency (employment by another healthcare provider). An alternative is self-supported training, which, however, is extremely rare.
There is a shortage of specialists in medical laboratory diagnostics in some regions in Hungary. This fact is taken into account by the health minister when he/she determines the number of trainees to be admitted, and allocates financial support. The authority – following consideration of the required number of specialists and the amount of available financial resources – assigns the number of trainees to be admitted for the given year. Enrollment to specialist training scheme is done by application. The number of trainees to be admitted is limited due to financial constraints. Admission examinations are justified by the need to select the best trainees. Trainees’ exams are assessed.
The training itself needs to be carried out at an accredited institutions, typically a university laboratory (1). All universities have to comply with a uniform system of requirements specified by a decree. The requirements for “medical laboratory diagnostics” training is published in the Official Gazette of the Ministry of Human Resources.
The training starts with a core program (lasting for 26 months). In practice, the core education can have a similar structure in several medical specialties. In the case of medical laboratory diagnostics the subtasks are as follows: emergency medicine (internal medicine, laboratory practice), specialties related to specific core education (molecular bio-pathology, clinical biochemistry), and courses. The 26 months of core education ends with an exam.
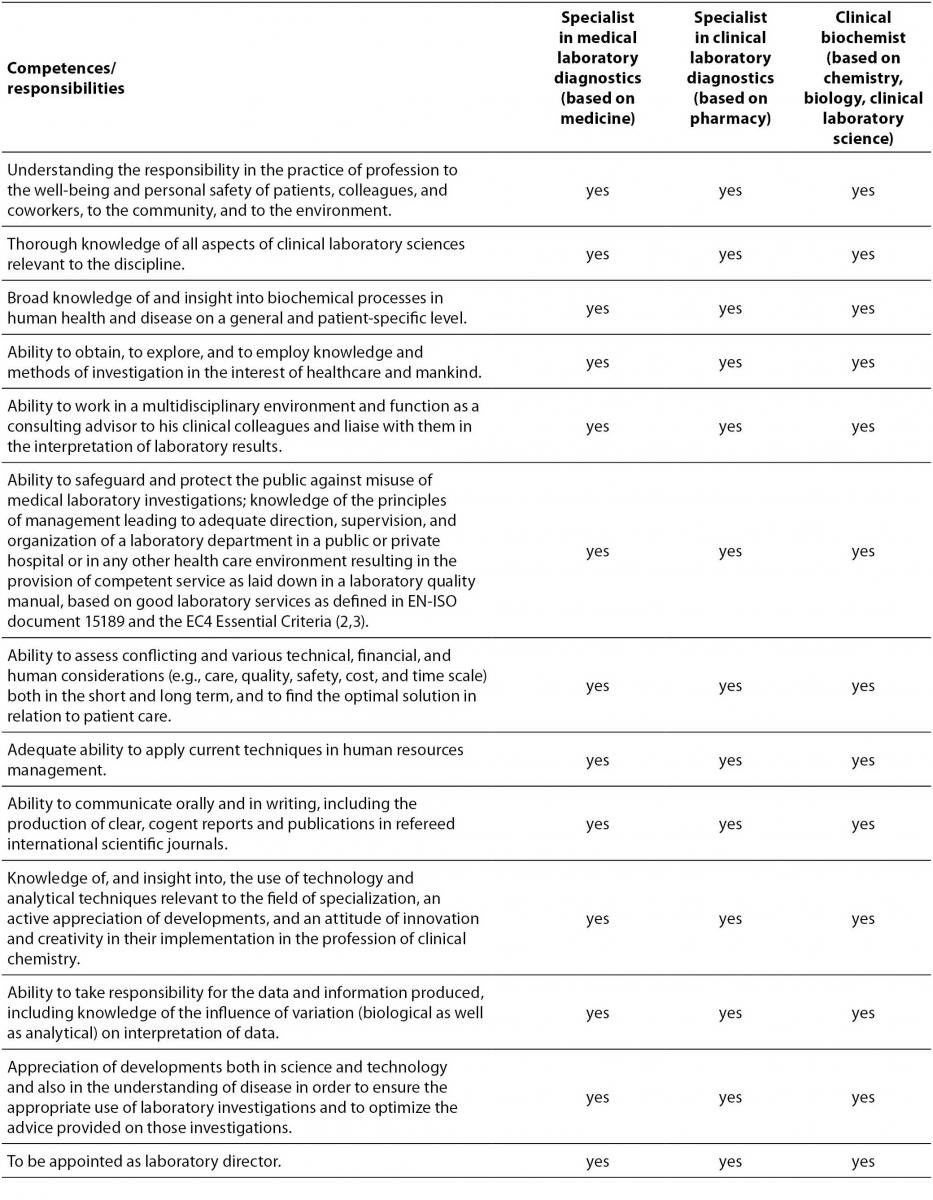
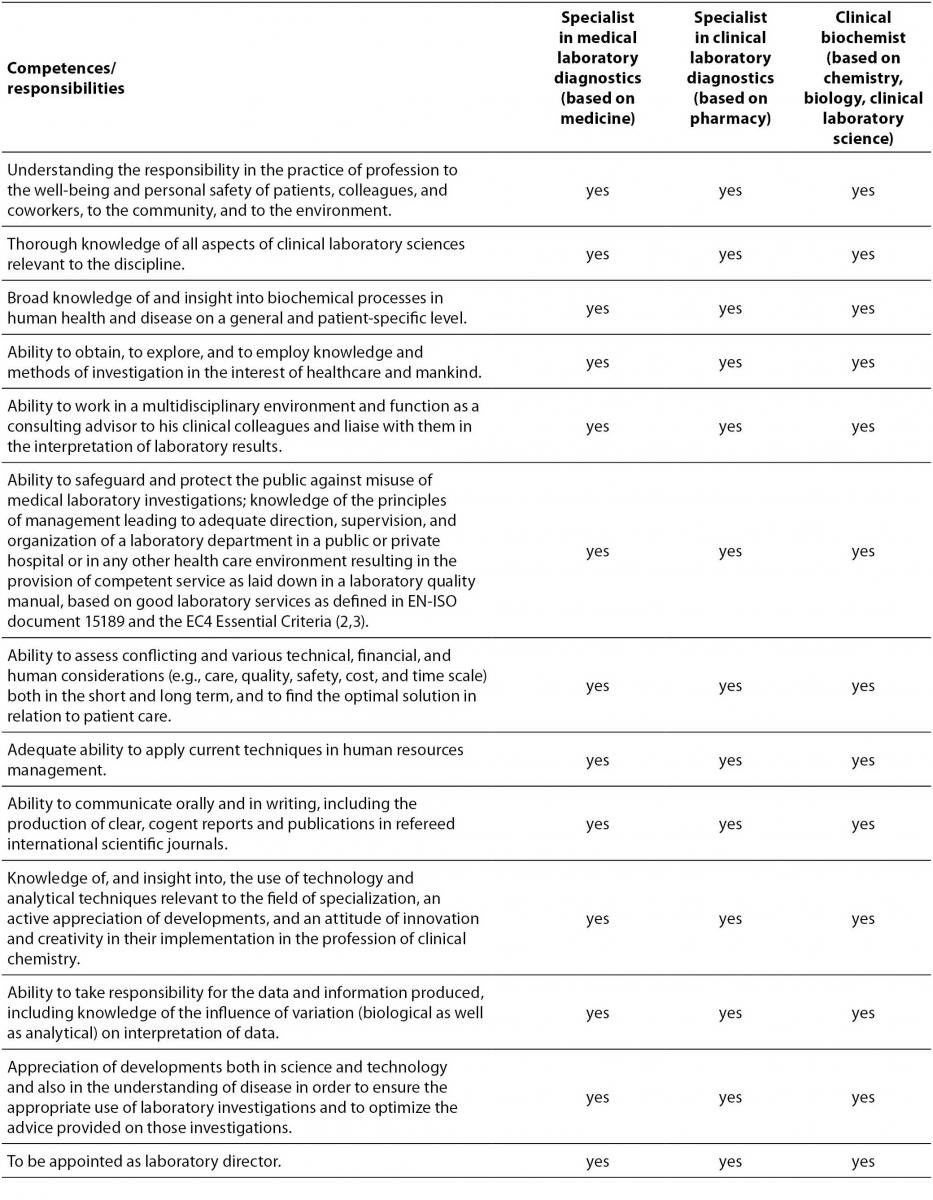
Specific education (34 months) follows the core training. It includes: hematology, hemostaseology, transfusiology, clinical microbiology, immunology, elective special courses, and a 12-month period of scientific education. Competencies of medical specialists are summarized in Table 1.
Table 1. Competences and responsibilities of laboratory specialists in Hungary.
When the trainee completed his/her training program, the university makes a recommendation to the National Examination Committee of the Council of Health Care Specialist Training to let the trainee take his/her specialist examination. The examination is taken in the presence of a panel made up of 3 independent examiners. In case of the medical laboratory diagnostics specialty, the exam has two parts: a practical exam (2-5 days), covering the various fields of medical laboratory practice (clinical biochemistry, hematology/hemostaseology, molecular genetics, clinical microbiology, and clinical immunology) and an oral theoretical exam – members of the exam panel are specialized and habilitated university professors.
Medical laboratory diagnostics can be a basis for the following secondary subspecializations (24-month further training times each): laboratory hematology and immunology, molecular genetic diagnostics.
To maintain their knowledge and keep up-to-date with science related to their specialization, specialists take part in further education courses, typically organized by universities. Achievement in further education is recorded as scores registered yearly by University Centers of Postgraduate Education. Specialists’ performance is evaluated every 5 years. To keep their licenses, specialists need to collect 250 points in a 5-year period. If they fail to do so, they can practice as specialists under supervision only. Requirement of CME/CPD (250 points in 5 years): theoretical scores organized CME training, local conferences, scientific research, individual training, long distance learning and practical scores: 20 points/year.
The system is kept up-to-date and accurately documented, and made available on the internet for medical (OFTEX) and pharmaceutical specialists (GYOFTEX). It also contains the upcoming further education events. At the end of the period, the specialist receives a certificate about his/her achievement from the Center of Postgraduate Education of the University, and he/she forwards this certificate to the national register, in order to keep his/her license.
The professors of laboratory medicine institutes can offer PhD programs for medical doctors. The staff of the Laboratory Medicine Institute at the Pécs University Medical School was also fairly active in the PhD programs in the past two decades: 14 individuals have received their PhD degree under supervision of the staff of the Laboratory Medicine Institute since 1993.
Undergraduate training of pharmacy students
Pharmacists are presently trained at either the four medical schools mentioned above. The curriculum includes obligatory, elective and optional subjects. During the first two years the students study basic subjects (chemistry, physics, biophysics, etc) and later these are changed to essential medical topics (anatomy, pathophysiology, internal medicine, clinical laboratory investigations, etc) and finally pharmaceutical subjects in details. At the University of Pécs clinical laboratory investigations, as a subject, is taught in the form of 24 hours of lecture during the first semester of the 5th year.
Postgraduate specialization of pharmacists (specialist in clinical laboratory diagnostics)
The training is accessible from 1999 by a government decree. The principles and the practice of specialist training are essentially the same as those for medical doctors. The schedule of training is as follows: 26 months of basic “core” training including 6 months clinical pharmacy and 6 months molecular biopathology; 12 months clinical biochemistry including 6 months clinical chemistry, 2 months TDM and toxicology, 2 months chromatography, 2 months diagnostic methods in endocrinology. After the final examination the candidates obtain a full license for clinical laboratory work. They supervise routine testing, validate results and introduce and/or develop new laboratory tests. All pharmacists with a specialty degree should join a continuous training program regulated by law (see above, described at the training of medical specialists). Pharmacists can also join university PhD programs and complete their studies obtaining a scientific qualification. Every university has its own PhD and habilitation regulation. Qualified candidates with outstanding research and continuous teaching activities may apply for the habilitation procedure as well.
Undergraduate education in laboratory medicine (BSc programs in medical laboratory analysis and medical research laboratory analysis)
The aim of the course is to train professionals who are able to perform and organize laboratory analytical work on their own in diagnostic and research laboratories. They will be able to manage sections of medical laboratories. Graduates will be familiar with modern methods of data analysis, and economics. They will have working knowledge in modern measurement methods, instrumentation, information technology, computing, and their applications in medical diagnostic and research laboratories. The duration of the BSc course is 8 semesters. In the first 4 semesters, students of both specializations study the same basic subjects. In the period of 5-8 semesters, the two programs teach different sets of basic subjects and specialized subjects. In the medical laboratory analyst program the emphasized subjects are the methodologies of clinical chemistry diagnostics, hematology, hemostaseology diagnostics, microbiological diagnostics, pathology, cytology and histology. In the medical research laboratory analyst program specialization takes place in basics of biochemistry, immunology, genetics, genomics and pharmaco-toxicology. In the last 2 semesters students have to do practical work at diagnostic or research laboratories of large hospitals or universities, respectively.
The competencies of a medical laboratory analyst are as follows: apply a thorough knowledge of chemistry, biochemistry, cell biology, microbiology, hematology, histology, cytology, computing and instrumental analysis, and be able to perform independent work in the fields of clinical chemical, isotope diagnostic, microbiological, histological, cytological and hematological diagnostics. A medical laboratory analyst is responsible for the management of the work of small laboratories or sections of laboratories directly and independently and is expected to be able to operate laboratory instruments, and keep them in appropriate working condition.
A medical research laboratory analyst is expected to apply a thorough knowledge of cell biology, genetics, molecular genetics, molecular biology, molecular morphology, immunology, cell culture, computing and instrumental analysis; to be able to work as an active contributor to modern research. Also, he/she should perform independent work in the main areas of modern analytical methods in a research laboratory, should be able to set up new methods with the aid of scientific literature, operate modern laboratory instruments, and systems of instruments, and supervise the work of cell-culture laboratories and animal facilities.
The BSc program in medical laboratory analysis is taught at the University of Pécs and at the University of Debrecen. The BSc program in medical research laboratory analysis is offered at the University of Debrecen.
Graduate education in laboratory medicine: MSc program in clinical laboratory science
In line with Directive 2005/36/EC of the European Union, graduates already having a BSc degree can be enrolled. Thus this master’s program of 3 semesters is a continuation of the 8-semester long BSc studies in medical laboratory analysis and medical research laboratory analysis. The aim of this MSc course is to train professionals who are familiar with the general and special rules and requirements of laboratory work, and they are able to perform active work in clinical research. They can perform, organize, control and evaluate trials of pharmaceutical and other therapeutic or diagnostic methods. They possess knowledge and skills which enable them to contribute to the development, preparation and manufacturing of pharmaceutical and diagnostic products. They are able to be up-to-date in scientific research. They have sufficient knowledge to enroll in a PhD program. MSc graduates are required to be familiar with the complex theoretical background and methodology of clinical research, the patho-biochemical background of the most important diseases, genetic, genomic, protein biochemical, immunological and pharmacological basis of clinical research, epidemiological and bio-statistical methods necessary to evaluate clinical research, the basics of research management and rules and bio-ethical guidelines of clinical trials. There is a period of research or epidemiological practical work incorporated in the course. To gain practical knowledge in planning and performing research, students take part in research projects in university research laboratories. According to the plans, the MSc program in clinical laboratory science is going to be launched in 2011 at the University of Pécs and at the University of Debrecen.
Postgraduate education in laboratory medicine for non-medical specialists: specialization in clinical biochemistry
Modern laboratory medicine requires the collaboration of medical and other professionals. Non-medical professionals have been able to specialize since as late as 2005. The conditions are laid out in a decree issued by the Ministry of Health. The decree refers to – in the framework of specialist education – clinical biochemists as primary specialization, and molecular biological diagnostic specialists as further specialization, built on the former, and also to the institutions of education. Regionally, Centers for Postgraduate Education, established in medical university towns, are in charge of the organization of the education. Candidates studying to obtain the specialization need to support themselves financially during the training. The candidate – who is required to have an MSc degree in biology, chemistry or clinical laboratory science – registers with a Regional Center for Postgraduate Education. The candidate’s workplace has to ensure that he/she can spend the full time with a teaching institution, or at least a part of this period at an accredited hospital laboratory. The duration of the specialist training is 48 months. Its structure is based on the practical training and the courses available at the accredited training institution:
- clinical biochemistry: 12 months;
- immunochemistry: 6 months;
- molecular genetic diagnostics: 5 months;
- therapeutic drug monitoring, toxicology: 3 months;
- chromatography, mass spectrometry: 3 months;
- hematology, hemostaseology: 3 months;
- elective specialty: 4 months;
- research project in laboratory diagnostics: 9 months;
- courses (elements of medical biochemistry, physiology, immunology, medical genetics, clinical chemistry, pharmacology, toxicology, research methodology, health care management, quality assurance, laboratory informatics and statistics): 2 months.
The exam for the clinical biochemistry specialization is made up of 2 parts, similarly to the specialty exam designed for medical doctors and pharmacists. Specialists in clinical biochemistry are qualified and authorized to execute laboratory diagnostic investigations, supervise technical staff, manage sections of laboratories of clinical biochemistry and its subspecialties (clinical chemistry, immunochemistry, endocrinology diagnostics, monitor drug levels, chromatography, mass spectrometry, toxicology and hematology), validate, publish and authorize the publication of results of the above mentioned investigations, set up laboratory methods and instruments, ensure their continuous operation, adapt and validate laboratory methods, carry out internal quality assurance, actively take part in quality assurance and development; manage external quality assurance, find and eliminate preanalytical, analytical and postanalytical errors, examine the operation of the laboratory from the point of view of management and human resources, training and further training of his/her subordinates, plan and enforce safety procedures in the laboratory, take part in further education, actively do scientific research in laboratory diagnostics and take part in professional public life.
To keep their knowledge up-to-date and learn new results of science and technology, the continuous further education of clinical biochemists (like that of medical specialists) is vital. Keeping a record of further education would need registration, but – due to lack of relevant legislation – registration is not possible for clinical biochemists. At present there is no mandatory method of scoring and assessing the professional practice of clinical biochemists.
Conclusions
In Hungary, the undergraduate, graduate and postgraduate education of laboratory specialists is a system with long-standing traditions; the quality is guaranteed by accreditation, and the rules are set by the government. The Institutes of Laboratory Medicine at the 4 medical schools – which are, at the same time, integral parts and laboratory service providers for the university hospitals - play a pivotal role in this process. For a certain part of the training program university departments may also involve laboratories of large teaching hospitals. Since Hungary joined the European Union in 2004, the training system has become fully harmonized with EC4 European Syllabus for Post-Graduate Training in Clinical Chemistry and Laboratory Medicine (2,3). A postgraduate qualification – a prerequisite of a full license in laboratory medicine – can be reached with a master’s degree either in medicine, pharmacy, chemistry, biology or clinical laboratory science. All postgraduate degrees in laboratory medicine – whether based on medicine, pharmacy, chemistry, biology or clinical laboratory science - fulfill the minimum standard for registration as a European Clinical Chemist (a total of 9 years of university and postgraduate study is required for all). A minimum of 4 years of postgraduate study after gaining a university degree is spent on specialist training in a laboratory in a medical environment approved and supervised by the national body. Only those specialists who have a postgraduate qualification in laboratory medicine and in addition to this also have a consecutive practice of at least 5 years as a specialist are eligible for the position of a laboratory director (Table 1).